Macrophages are a critical part of our immune system. They patrol our tissues, and when they encounter debris or invaders such as bacteria and parasites, they engulf the particles and destroy them. But if, in the course of tuberculosis, these infected macrophages die through a process called necrosis, in which the cells burst open, then the engulfed bacteria are released back into the extracellular environment where they can grow unrestricted.
Lalita Ramakrishnan’s group, in the University of Cambridge Molecular Immunity Unit that is housed within the LMB, has identified a novel form of such macrophage death which is pathological in TB, and have identified already-available, safe, inexpensive drugs that can be used to intercept this cell death, and thereby potentially save lives.
Lalita’s group had previously found that zebrafish with an increased expression of the enzyme leukotriene A4 hydrolase were more susceptible to TB. They observed that the resultant excess of its product, leukotriene B4, increased bacterial growth. This finding was very surprising, as it was expected that leukotriene B4, a well-known inflammation-promoting lipid mediator, should be protective against infection, rather than support bacterial growth. The team determined that this was due to increased amounts of leukotriene B4 triggering an excess production of the immune molecule TNF. Importantly, TNF at optimal levels is required to protect against TB, but it is the excess that is detrimental and leads to macrophage death through necrosis. Francisco Roca and other members of Lalita’s group have now identified the mechanism by which excess TNF worsens disease pathology.
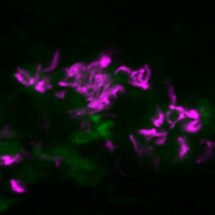
For this study, the scientists infected zebrafish larvae with mycobacteria, under conditions of normal and high TNF, and monitored the sequence of events that led to the necrosis of the infected macrophages. In doing so, they identified a complex pathway with new roles identified for already well-studied proteins and involving signalling between multiple compartments within the cell: mitochondria, lysosomes, and the endoplasmic reticulum. Importantly, this necrosis pathway is also potentially linked to susceptibility to human TB caused by a common genetic variant in leukotriene A4 hydrolase.
By identifying the pathway by which excess TNF leads to macrophage death and increased bacterial growth, this work identifies potential new host-targeting treatments – which include commonly used drugs for conditions such as high blood pressure – for TB. Because these drugs target host processes that the bacterium depends on, they are expected to be useful in both drug-sensitive and drug resistant TB. Drug resistant TB is a major public health problem and a formidable obstacle to effective TB care and prevention globally.
This study was funded by the Wellcome Trust and the US National Institutes of Health.
Further references:
TNF induces pathogenic programmed macrophage necrosis in tuberculosis though a mitochondrial-lysosomal-endoplasmic reticulum circuit. Roca, FJ., Whitworth, LJ., Redmond, S., Jones, AA., Ramakrishnan, L. Cell 178: 1-18
Lalita’s group page