Mammoth team effort enables use of live virus for rapid responsive COVID-19 research into SARS-CoV-2 infection and immunity that could help future vaccine development
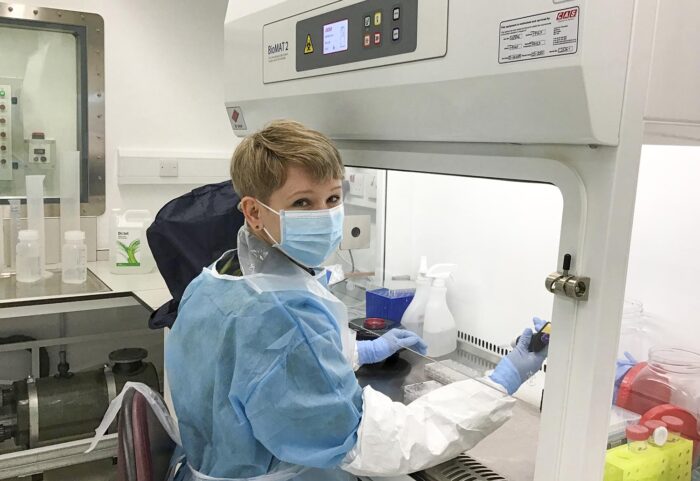
© Anna Albecka-Moreau
When the LMB buildings closed in March, Leo James’ research group quickly sprang into action refocusing their virology expertise to COVID-linked research. But to fully realise the potential of their skills, they needed access to specialist laboratory space in order to work on the live SARS-CoV-2 virus.
Work with pathogenic viruses must take place within Containment Level 3 (CL3) laboratories under strict safe working practices to ensure a high level of protection for those working on the virus. A suitable laboratory already existed in the LMB, but it was not yet operational.
To enable vital research using live virus by Leo’s group and others, a team including those with expertise in research safety, building management systems and virus research was rapidly assembled to fast-track opening of the LMB’s CL3 lab.
In tandem, leading virologists and experienced CL3 users from across Cambridge, including Ian Goodfellow and Mark Wills, got together to ensure training expertise was shared to equip scientists with the practical skills needed to work with the live SARS-CoV-2 virus.
After a mammoth team effort, the LMB’s CL3 laboratory was opened within just three months. The first virus samples arrived from Cambridge University Hospital on the very same day, and results from experiments using live virus have already contributed to two research publications, with more in the pipeline.
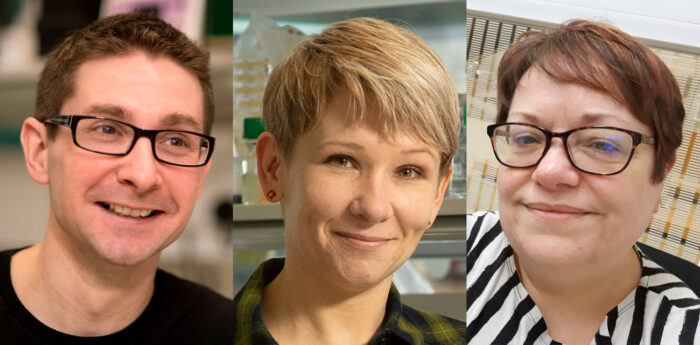
Here, Leo James, Anna Albecka-Moreau, a virologist in Leo’s group, and Jillian Deans, LMB Head of Health and Safety, share further details about opening the CL3 laboratory and the research this is enabling:
What is your prior relevant experience?
Leo: My group looks at antibody immune responses, specifically how antibodies prevent viral infection. Our work focuses on a cytosolic antibody receptor called TRIM21. We investigate how TRIM21 uses antibodies to block infection inside the cell.
Prior to the pandemic we were investigating the role of antibodies that target nucleoprotein – the protein that wraps up the viral genome within the virus particle – in viruses such as flu, whether they might have a role in blocking infection, and whether TRIM21 was involved in that. When the pandemic hit, we applied these same questions to SARS-CoV-2.
Anna: I am a molecular virologist and have worked with different enveloped viruses for many years, including at Level 3 Containment, so my prior skills and knowledge were very useful when setting up the safe work practices.
Jillian: Although I’ve never worked in a CL3 lab, my previous experience as a Specialist Inspector for HSE and as Biological Safety Adviser at both the University of Liverpool and UCL meant I had seen a lot of different CL3 set-ups as well as having being hands-on getting CL3 laboratories operational.
I also had access to a really great network of biosafety colleagues across the UK and Europe through membership of the Institute of Safety and Technology in Research (ISTR) and the European Biosafety Association (EBSA) – if I didn’t know the answer to a question, I always knew someone who could help.
What did opening the CL3 lab involve?
Anna: The CL3 lab had been a work in progress for many years but with the start of the pandemic many members of LMB, particularly Jillian and Stephen Holmes (Head of Estates), worked really hard to make the lab functional within just 3 months. Leo put everybody together and made this process roll really fast.
Leo: It really has been a massive team effort involving LMB Health and Safety, Estates and Facilities and Lab Services teams, Chris Tate (LMB’s Biological Safety Officer), Laura Whitworth and Emma Heath from the Molecular Immunity Unit (University of Cambridge unit based within the LMB), and Anna and myself from my group.
From April we had weekly meetings, usually for about an hour and a half, just to give out the tasks for everyone to do. It was hugely intensive.
Jillian: As with any project like this, we had a lot of issues to cover from being able to do the planned science as well as making sure the laboratory met all legal requirements. Meeting on a weekly basis meant we could maintain momentum and share the work-load – it really helped being part of such a knowledgeable and experienced multi-disciplinary team.
Leo: Very early on we realised that we not only needed access to CL3 labs, but also training with aerosolised pathogens. Fortunately, virologists and CL3 experts in labs across Cambridge were already getting together to ask: “How are we going to provide CL3 training to support COVID work?”.
Ian Goodfellow from the Pathology Department played a key role in getting clinicians and scientists together, sourcing virus, and establishing some of the early assays.
The first wave of training involved five people who were experienced CL3 virologists and had some prior experience with respiratory pathogens – including Anna in my lab. Mark Wills from the Department of Medicine (University of Cambridge) oversaw the training and provided the CL3 labs to train this initial group.
Anna: I was a member of the first group of SARS-CoV-2 trained virologists in Cambridge. Our team established procedures to work with the virus, adapting TB protocols used at the Department of Medicine. During the training I wrote all the Standard Operating Procedures (SOPs) to establish safe assays for LMB SARS-CoV-2 work. This was greatly aided by input from Chris Tate.
Jillian: Having completed all the necessary paper-work for HSE and following a number of dry runs and final checks on equipment, the team agreed that work with the live virus could start – the final hurdle being to safely transport it to the building from the Department of Medicine. When I heard from Anna that the virus had arrived and been safely unpacked in the CL3, I did breathe a huge sigh of relief that we had finally got there.
What has research using the live virus enabled?
Anna: The lab opened on 22nd of June and I started my first COVID experiment that day. My first exciting results came from a collaboration with Madeline Lancaster’s lab, where I inoculated brain organoid tissues to investigate what cell types are permissive to infection. Together with Laura Pellegrini we showed that SARS-CoV-2 can infect cells in the brain-CSF barrier, which leads to leakage through this important protective layer.
Donna and Guido in our group were working very hard during the lockdown and had generated nice results, in collaboration with Sean Munro’s lab, on how the viral spike protein is processed by a host protease. I was able to add a few experiments using live virus to confirm some of these findings, which have now been published (pre-print: peer review in progress).
But my main project is to look if the virus can be neutralised inside cells by the TRIM21 mechanism that our lab is interested in.
Leo: In the context of COVID-19, everyone is looking at the spike protein – which coats the outside of the virus particle and mediates cell entry – and how spike antibodies stop the virus getting into cells.
However, if you look at the immune responses that people infected with the COVID-19 virus are making, the strongest antigen – the part of the virus you make most antibodies against – is the nucleoprotein.
Anna: But, as nucleoprotein is hidden inside the virus particle, we don’t understand if these antibodies against nucleoprotein have a role in immunity. Our study can help answer this question. This is important because we need to know whether to include nucleoprotein in vaccines.
Leo: We’ve developed an intracellular neutralisation assay based on our Trim-Away technology that enables us to artificially deliver antibodies against nucleoprotein into cells. In the CL3 lab we can then infect the cells with SARS-CoV-2 and see whether the virus is able to replicate or is blocked by the nucleoprotein antibody.
Anna: My initial results using the TRIM21 neutralisation assay are very promising. I have also started working on a new project with Radu Aricescu and Jan Löwe to test new vaccine candidates. And Charlotte Passemar from Andres Floto’s group in the Molecular Immunity Unit will soon start to use a unique and very innovative lung-on-chip model to emulate SARS-CoV-2 infection and test different treatments.
What next?
Leo: We will continue with our COVID-linked research: we are doing something we are uniquely equipped to do and I feel we can make a really useful contribution.
Anna: I think I will continue working with SARS-CoV-2 for a while. We are in urgent need of more accessible, oral antivirals and these have to be tested in cell culture first.
Our facility can be of use to pharmaceutical companies working on new treatment strategies and fast diagnostic tests and we are already in contact with several of them. We will also continue our project on TRIM21-dependent neutralisation.
In the future we would also like to make use of the new facility to support our ongoing HIV work.
Jillian: Now the laboratory is open, we are well on the way to starting the planned work with TB by both the Ramakrishnan and Floto groups, including using the lung-on-chip model to understand the immune response to Mycobacterium tuberculosis and develop new drug treatments. Leo also has plans for other CL3 work so this laboratory will be a valuable resource for LMB in the coming years.
Further references
LMB joins the fight against COVID-19
Leo’s group page
Ian Goodfellow’s group page
Mark Wills’ group page
SARS-CoV-2 disrupts the brain barrier in human organoids
Furin cleavage of SARS-CoV-2 Spike promotes but is not essential for infection and cell-cell fusion (pre-print – not yet peer reviewed)