Establishing how brain temperature varies normally in four dimensions could transform how we diagnose and manage several brain disorders, and our understanding of how the brain works
Brain cell function is profoundly sensitive to changes in temperature, yet we know so little about what our brain temperature should be. Human brain temperature is rarely measured directly because this requires intrusive methods. Consequently, our knowledge of human brain temperature is built upon studies of brain-injured patients, where brain monitoring probes allow precise measurement from one location in the brain. However, brain injury can affect brain temperature, and interpreting brain temperature data from patients is difficult without a reference range from healthy human brains to compare these data with.
A cutting-edge brain imaging technique called magnetic resonance spectroscopy (MRS) now allows researchers to measure brain temperature non-invasively. Exploiting this technique, a study led by Nina Rzechorzek from John O’Neill’s group in the LMB’s Cell Biology Division, in collaboration with Edinburgh Imaging at The University of Edinburgh, has revealed the remarkable extent to which temperature varies across brain regions and over time in healthy adults.
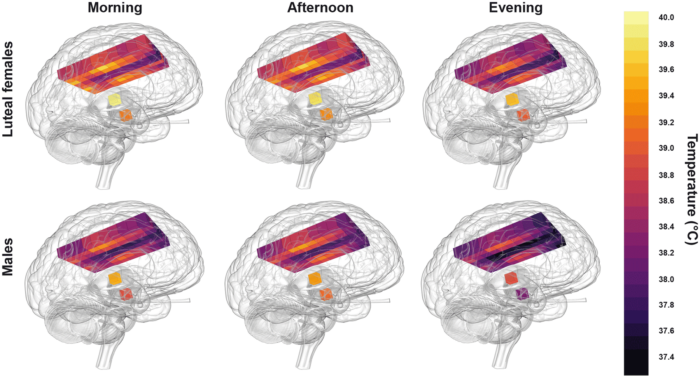
Collaborating with neurocritical care specialists at NHS Lothian, Edinburgh, and Addenbrooke’s Hospital, Cambridge, the group drew upon the Europe-wide CENTER-TBI database of patients with traumatic brain injury to find patients who had their brain temperature measured continuously and directly in intensive care. To compare these data with healthy brains, the researchers recruited 40 healthy volunteers (20 males, 20 females, aged 20-40 years) for non-invasive brain thermometry. They used MRS to measure temperature in 82 brain locations in the morning, afternoon, and late evening, which included the first thermal imaging of the hypothalamus (the brain region responsible for regulating temperature and the body clock). Assisted by the LMB Visual Aids department, the results were incorporated into HEATWAVE, a freely-available 4D map of healthy human brain temperature.
The key finding was that healthy human brain temperature varies far more than previously assumed – by age, sex, menstrual cycle, brain region and, most importantly, by time of day. Noting that a daily brain temperature rhythm was often absent in patients after traumatic brain injury, the team found a striking relationship between the presence of this rhythm and survival in intensive care. They concluded that daily brain temperature variation is likely to hold greater clinical value than absolute brain temperature and that individual patient factors should be considered when interpreting brain temperature data.
Astonishingly, parts of the healthy human brain routinely exceeded 40°C, suggesting that such temperatures do not immediately impair brain cell function. These higher temperatures were most often observed during the afternoon in core brain regions of females who were in the post-ovulation phase of their menstrual cycle. In addition, the group found that brain temperature increased with age. This finding was quite unexpected given the confined age range (20-40 years) of the volunteers and the lack of data describing this phenomenon in any other species. An age-related temperature increase suggests that the brain’s capacity for cooling deteriorates with age. This raises an important question to address in further research of whether progressive failure to cool the brain could influence the development of age-related brain disorders such as dementia.
Healthy human brain temperature clearly decreased at night in both males and females. Such time-of-day variation might explain diurnal changes in cognitive performance and help us understand how brain temperature interacts with sleep. We already know that sleep disruption—for example during shift work or jet lag—has a negative impact on cognitive performance and mental health and this study has now provided a catalyst for exploring the relevance of brain temperature to several challenging brain disorders. Moreover, HEATWAVE represents a vital pre-pandemic snapshot of human brain temperature that can support studies on the impact of emerging infectious disease and climate change on brain health.
As for any patient parameter, changes in brain temperature can be fully exploited as a diagnostic or prognostic tool only if abnormal deviations can be distinguished from normal variation over time. Although the findings from this work are largely correlative, they have addressed a fundamental knowledge gap about human brain temperature and thus redefined how it might be useful in the critical care setting. An important goal of future work is to address whether abnormal daily brain temperature rhythmicity can serve as an early biomarker of neurodegeneration.
Beyond the clinic, these new data challenge scientists to review how human brain cells are grown and studied in the lab. HEATWAVE is already being used to test how daily variation in human brain temperature interacts with molecular ‘clocks’ within human brain cells, aiming to better understand temperature as a circadian timing cue and probe the true thermodynamics of brain function.
This work was funded by UKRI MRC, Hannelore Kohl Stiftung, OneMind, Integra LifeSciences Corporation and NHS Lothian Research and Development Office. Data obtained in the context of CENTER-TBI was funded by EC grant 602150 and supported by the European Union’s 7th Framework program (FP7/2007-2013).
Further references
A daily temperature rhythm in the human brain predicts survival after brain injury. Rzechorzek, NM., Thrippleton, MJ., Chappell, FM., Mair, G., Ercole, A., Cabeleira, M., The CENTER-TBI High Resolution ICU (HR ICU) Sub-Study Participants and Investigators, Rhodes, J., Marshall, I., and O’Neill, JS. Brain.
John O’Neill’s group page
HEATWAVE
Previous Insight on Research articles
How cellular clocks within heart cells coordinate daily cardiac rhythms
How eating feeds into the body clock