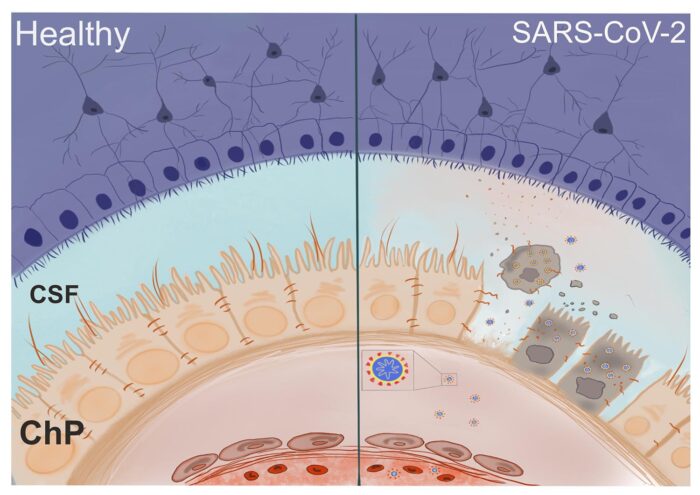
The virus responsible for COVID-19 is able to infect choroid plexus cells, causing leakage through the brain-CSF barrier, which may lead to long-term neurological complications
COVID-19 is primarily associated with respiratory effects, but there have been increasing reports of neurological symptoms alongside these. The cause of these complications, whether by direct infection of brain cells or by indirect inflammatory effects, is currently unknown. Using brain organoids, Madeline Lancaster’s group, in the LMB’s Cell Biology Division, has found that the virus can disrupt the blood-CSF barrier, which may lead to a neuroimmune response and long-term complications.
Madeline’s group have developed brain organoid models to study development, function, and disease. One brain tissue they wanted to study is the choroid plexus (ChP), which produces and secretes cerebrospinal fluid (CSF) and forms a barrier between the CSF that bathes the brain and the blood. To do this, they recently developed a brain organoid model of the ChP and found it capable of forming a tight barrier similar to the blood-CSF barrier in the human brain with the potential to predict whether drugs can access the brain.
Madeline’s group realised this model could also be useful to investigate whether SARS-CoV-2, the virus responsible for COVID-19, is able to infect cells in our brain, so they looked to see which cells have ACE2, the receptor needed for SARS-CoV-2 entry, on their surface. They found that ChP cells express ACE2, but neurons and other cell-types don’t.
Laura Pellegrini, a member of Madeline’s group, and Anna Albecka-Moreau, a member of Leo James’ group, then challenged the brain organoids with pseudoviruses carrying the SARS-CoV-2 spike protein and with live virus to see which cells the virus could infect. They found that the virus is able to infect and produce new virus inside ChP epithelial cells, but neurons and glia were not susceptible to infection.
Following infection they saw that some proteins responsible for forming the tight contacts between cells were mislocalised, allowing brain barrier leakage. This weakening of the CSF-blood barrier could allow entry of pathogens, immune cells, and cytokines into the cerebrospinal fluid and brain, potentially leading to neuroinflammation.
This work shows that, in more severe cases where the virus has entered the blood from the lungs, it is possible for SARS-CoV-2 to enter the brain. Although the virus is unlikely to propagate in brain cells, the damage it causes at the brain barrier may lead to cytokine and immune cell invasion and result in long-term neurological symptoms such as chronic fatigue. Knowledge of which cells are more susceptible to SARS-CoV-2 infection is important for design of more targeted therapeutic approaches and understanding the long-term effects of infection.
The work was funded by UKRI MRC.

Personal perspectives of COVID-19 research
We are accompanying Insights on Research that cover COVID-19 research with interviews with the scientists who carried out the work, to give some perspective of the experiences of transitioning to COVID-19 research and working at the LMB during the height of the ongoing pandemic. One member of Madeline’s group who led this research on the SARS-CoV-2 infection in choroid plexus organoids, Laura Pellegrini, describes why she ended up doing this work and what it was like working on this project.
What is your normal research focus?
My research is focused on the development and function of a particular region of the brain called the choroid plexus, which secretes the cerebrospinal fluid and acts as a brain barrier. To study this brain region, I use stem-cell derived cerebral organoids.
Why did you change focus to work on COVID-linked research?
It recently became clear that there are neurological symptoms associated with COVID-19 and we have no idea of their long-term implications. With the excellent support of my supervisor, Madeline Lancaster, and the expertise of Leo James’s group we decided to take advantage of our new organoid model to study SARS-CoV-2 entry into the brain, whether the virus can directly infect neuronal cells and its potential implications in the brain barrier damage.
How might this research make a difference to the pandemic outcome?
It’s important to do this research because finding whether the virus can directly infect neural cells or whether the neurological symptoms observed are the cause of an exaggerated immune reaction will help clinicians to choose the right treatments and potentially prevent long-term adverse effect, such as chronic fatigue that was reported for other similar coronaviruses.
What have you missed when working in the lab during the pandemic?
I really missed the social interactions with my colleagues and having lunch together in the LMB canteen, the animated discussions over various topics, the LMB social events in general.
Was collaboration important?
Yes, absolutely. The collaboration with Leo James’s group was crucial for this study. They provided all the key reagents for the project and Anna Albecka was performing the riskiest part of handling live SARS-CoV-2 to infect our organoids. Without this collaboration this project would not have been possible.
What have been the challenges?
The challenges, when working with such an infectious pathogen, have been to rethink how to perform certain experiments in order to meet the safety measures in place and this limited some of the procedures we normally use in the lab such as the use of sharp tools to extract the fluid inside organoids for analysis.
What next? Will your involvement in COVID research continue or are you returning to your normal research focus?
There is still a lot we don’t know about this virus and it’s important to continue the basic, fundamental research. For the next few months, I plan to continue the investigation of the biological changes in the choroid plexus after SARS-CoV-2 infection and whether the virus can spread in the cerebrospinal fluid.
Further references
SARS-CoV-2 infects the brain choroid plexus and disrupts the blood-CSF-barrier. Pellegrini, L., Albecka, A., Mallery, DL., Kellner, MJ., Paul, D., Carter, AP., James, LC., Lancaster, MA. Cell Stem Cell https://doi.org/10.1016/j.stem.2020.10.001
Madeline’s group page
Leo’s group page
LMB joins the fight against COVID-19
Previous Insight on Research
Brain organoids with the potential to predict drug permeability